Local Perfusion MRI in Acute Stroke
Purpose: Demonstration of “local” perfusion, i.e. all blood flow within a region whether supplied antegrade or delayed and dispersed through the collateral network, containing information regarding collateral supply, infarct growth rate, and flow augmentation treatment response in acute stroke.
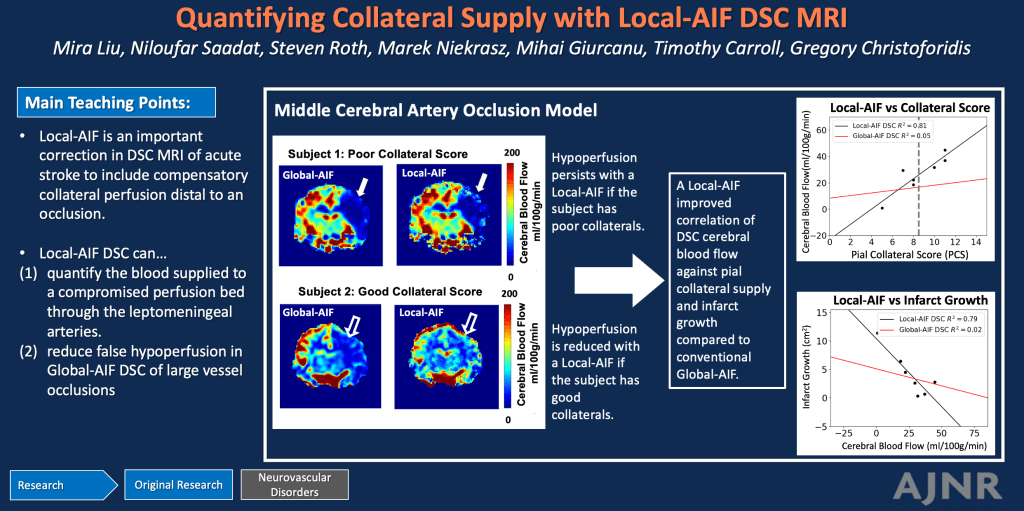
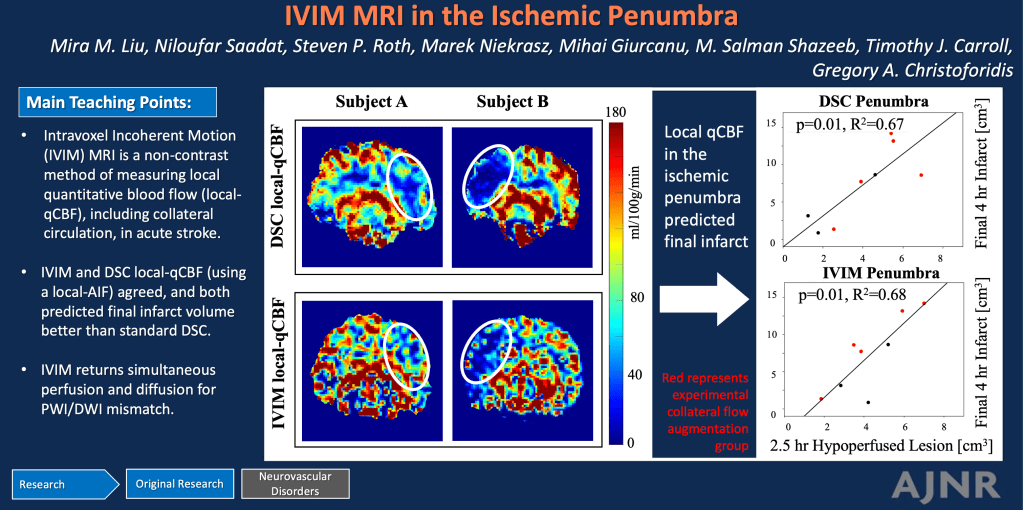
Methods and Materials: Two methods of local perfusion (i.e. “local” quantitative cerebral blood flow, qCBF in ml/100g/min) are included: 1) dynamic susceptibility contrast (DSC) MRI with a local arterial input function for delay and dispersion correction , 2) intravoxel incoherent motion (IVIM) which is by nature independent of blood flow path or delay. Standard perfusion is included with DSC using a traditional global-AIF. These are compared to standard AIF-dependent DSC perfusion. Experiments in a model of middle cerebral artery occlusion were performed and native collateral circulation was quantified via x-ray DSA 30 minutes post-occlusion. Some also underwent flow-augmentation aimed to boost collateral supply to the affected territory. DSC MRI was acquired 2.5hrs post-occlusion and post-processed first with a standard global-AIF, and second with a Local-AIF. A subset with IVIM MRI was acquired and post-processed to returned local-qCBF from fD*. Infarct volume was measured with standard DWI at 2.5hrs and 4hrs post-occlusion.
Results: (1) The degree of collateralization at x-ray correlated more strongly with DCS local-qCBF in the ischemic penumbra (R2 = 0.81) than with standard DSC qCBF (R2 = 0.05); inclusion of delayed and dispersed flow for a “local” DSC perfusion demonstrated ability to capture collateral flow in the affected territory. (2) IVIM local-qCBF in the penumbra correlated with DSC local-qCBF (R2=0.69); the local nature of IVIM, as it is intravoxel rather than tracer-based, may by its very nature automatically include all perfusing blood, including collateral flow, in the affected territory. (3) Correlation was weaker between IVIM and standard DSC (R2=0.13); standard DSC may have false hypoperfusion when it does not account for a robust collateral supply, while IVIM inherently includes it. (4) Both DSC and IVIM local-qCBF predicted final 4hr infarct volume (R2=0.78, R2=0.61 respectively) while standard DSC was a weaker predictor (R2=0.12). The volume of hypoperfused lesion from DSC and IVIM local-qCBF both predicted final infarct volume with good sensitivity and correlation (slope=2.08, R2=0.67, slope=2.50, R2=0.68 respectively). As collateral flow can delay or slow infarction, inclusion of collateral flow using “local” perfusion imaging may improve prediction of infarction.
Conclusions: In acute stroke, local perfusion with Local-AIF DSC or IVIM can assess tissue status and collateral supply in acute stroke more accurately than conventional Global-AIF DSC. These findings support using local perfusion that includes delayed and dispersed retrograde flow when imaging the affected territory of acute stroke. Further, as IVIM is non-contrast, it can allow longitudinal and repeated measurement of local-qCBF may include collateral circulation, simultaneous perfusion and diffusion images, and improve prediction of infarct growth.
List of some publications relevant to this topic:
Local-Perfusion MRI in Stroke
M. Liu et al. A Method for Imaging the Ischemic Penumbra with MRI using IVIM Am J Neuroradiol, 2025
M. Liu et al. Quantification of Collateral Supply with Local-AIF Dynamic Susceptibility Contrast MRI Predicts Infarct Growth Am J Neuroradiol, 2025
J. Zimmermann et al. Intravoxel incoherent motion imaging in stroke infarct core and penumbra is related to long-term clinical outcome. Sci Rep, 2024
C. Federau et al. Collateral blood flow measurement with intravoxel incoherent motion perfusion imaging in hyperacute brain stroke. Neurology, 2019.
C. Federau et al Intravoxel incoherent motion perfusion imaging in acute stroke: initial clinical experience. Neuroradiology, 2014
S. Suo et al. Stroke assessment with intravoxel incoherent motion diffusion-weighted MRI. NMR Biomed, 2016
G. Zhu et al. Comparison of MRI IVIM and MR perfusion imaging in acute ischemic stroke due to large vessel occlusion. Int J Stroke, 2020
Quantitative Local-Perfusion MRI post-processing methods
TJ. Carroll et al. Automatic Calculation of the Arterial Input Function for Cerebral Perfusion Imaging with MR Imaging Radiology, 2003
YI. Jeong et al. Absolute quantitative MR perfusion and comparison against stable-isotope microspheres. Magn Reson Med, 2019.
JJ. Mouannes-Srour et al. Correction for arterial-tissue delay and dispersion in absolute quantitative cerebral perfusion DSC MR imaging. Magn Reson Med, 2012
M. Liu et al. Quantitative perfusion and water transport time model from multi b-value diffusion magnetic resonance imaging validated against neutron capture microspheres. Journal of Medical Imaging, 2023.
Collaterals and flow augmentation in stroke
N. Saadat et al. Influence of simultaneous pressor and vasodilatory agents on the evolution of infarct growth in experimental acute middle cerebral artery occlusion.” J Neurointerv Surg, 2020.
M. Liu et al Augmentation of Perfusion with Simultaneous Vasodilator and Inotropic Agents in Experimental Acute Middle Cerebral Artery Occlusion: A Pilot Study. J Neurointerv Surg, 2022.
GA. Christoforidis et al. Impact of Pial Collaterals on Infarct Growth Rate in Experimental Acute Ischemic Stroke Am J Neuroradiol, 2016.
DS. Liebeskind. Collateral Circulation. Stroke, 2003.
SM. Uniken Venema et al Cerebral Collateral Circulation in the Era of Reperfusion Therapies for Acute Ischemic Stroke. Stroke, 2022.
GA. Christoforidis et al Effect of early Sanguinate (PEGylated carboxyhemoglobin bovine) infusion on cerebral blood flow to the ischemic core in experimental middle cerebral artery occlusion. J Neurointerv Surg, 2022
MS. Shazeeb et al Novel Oxygen Carrier Slows Infarct Growth in Large Vessel Occlusion Dog Model Based on Magnetic Resonance Imaging Analysis. Stroke, 2022